Public-private partnership is still a misunderstood concept particularly when applied to the ‘soft side’ of development projects (e.g., for health and social development).
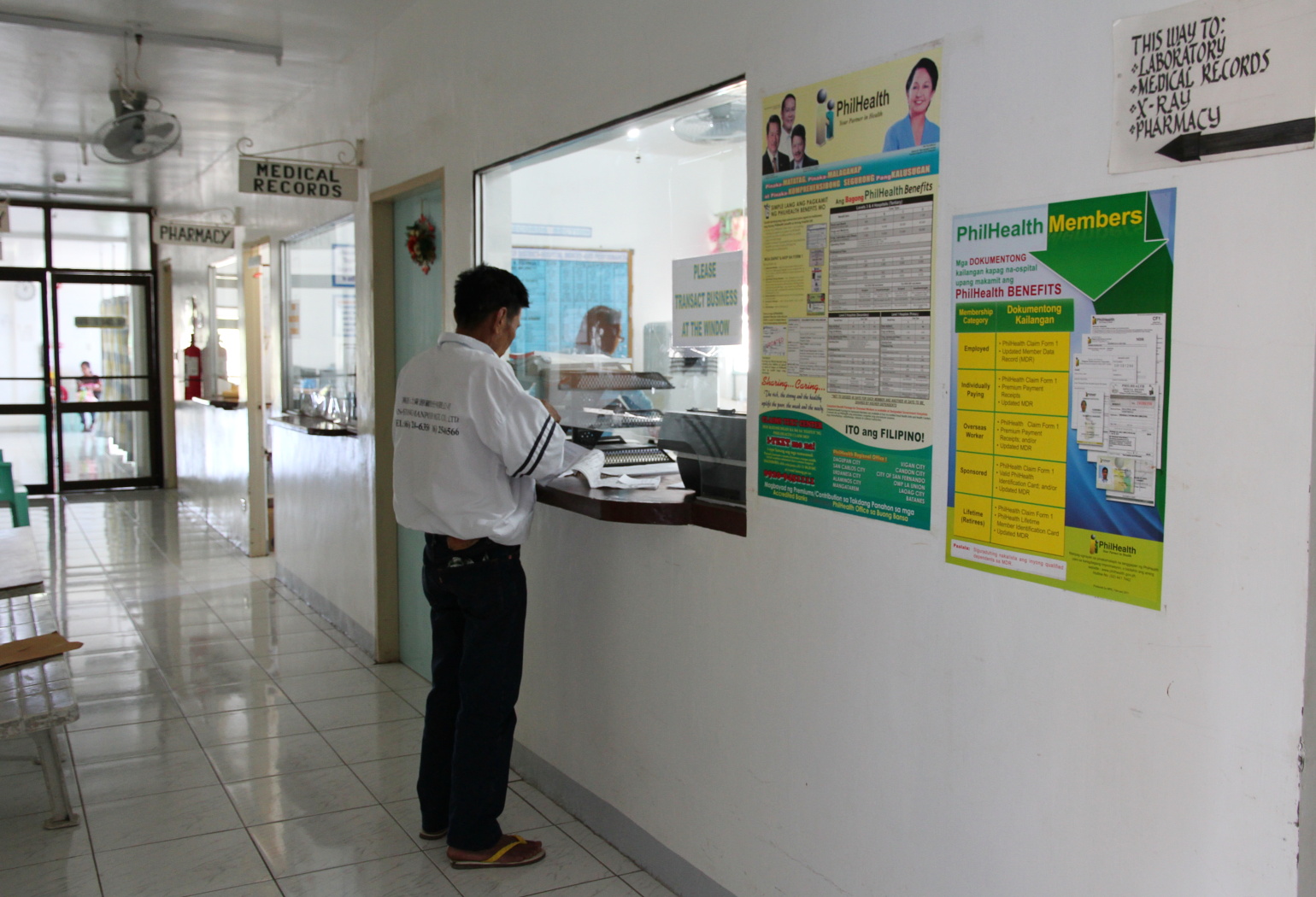
PPP in health allows faster and more efficient procurement, which addresses perennial inventory gaps/issues in many public hospitals. [Image by M. Velas-Suarin]
Some of the negative perceptions include higher costs of health services, relegating of responsibilities to the private sector (or even describing it as outright privatization!), and retrenchment of government employees. If we will remember, these are some of the issues that were hurled against previously-planned PPP projects in health not just in the Philippines but in other locations worldwide.
The negative perceptions may indeed be addressed through clearer messaging and social marketing–e.g., that PPPs (at least, when done properly) is about harnessing partnerships where the public sector benefits from the efficiency of the private sector. We all know that government procurement laws–while rooted from good intents–tend to slow down purchasing, leading to stocking and inventory gaps and problems, for example, in government pharmacies.
More importantly, positive experiences from good models will speak for themselves. There are already good and best practices from all over the world. The Philippine health sector should do more in terms of clarifying the issues and building new PPP in health projects, particularly with LGUs. After all, we will not really know if something is indeed good (or bad) for us if we have not really experienced it.
The following are just some of the more important things that PPP in health projects should consider:
- How to ensure that PPP arrangements will effectively support public health goals and be economically sound
- How to ensure adequate and responsive legal and policy environment
- How to establish and institutionalize PPP financial mechanisms that cover disbursements and utilization of, and reporting on public-private funds
- How to effectively monitor performance, anchored on the need to reflect benefits for the community
- How to deepen public acceptance through social marketing.
PPPs are not supposed to be the end-all-be-all solution for complex issues and problems in health. There are indeed public hospitals that are better managed in the traditional way. However, PPPs, when applied and implemented correctly, can certainly help achieve intended health outcomes and universal health care. (M. Velas-Suarin)
*These key considerations had been lifted from the author’s earlier work titled, Five Applications in PPP in Health, co-written with Dr. Juan Ma. Pablo Nañagas, and developed under the ADB TA 7257 PHI: PPP in Health. A copy of the work is found under “Resources.”
__________
Disclaimer: This article is entirely the work of the author (unless stated otherwise) and does not represent the opinions or policy statements of HOPE, Inc., its officers, staff, and partners, and other third-party organization.
